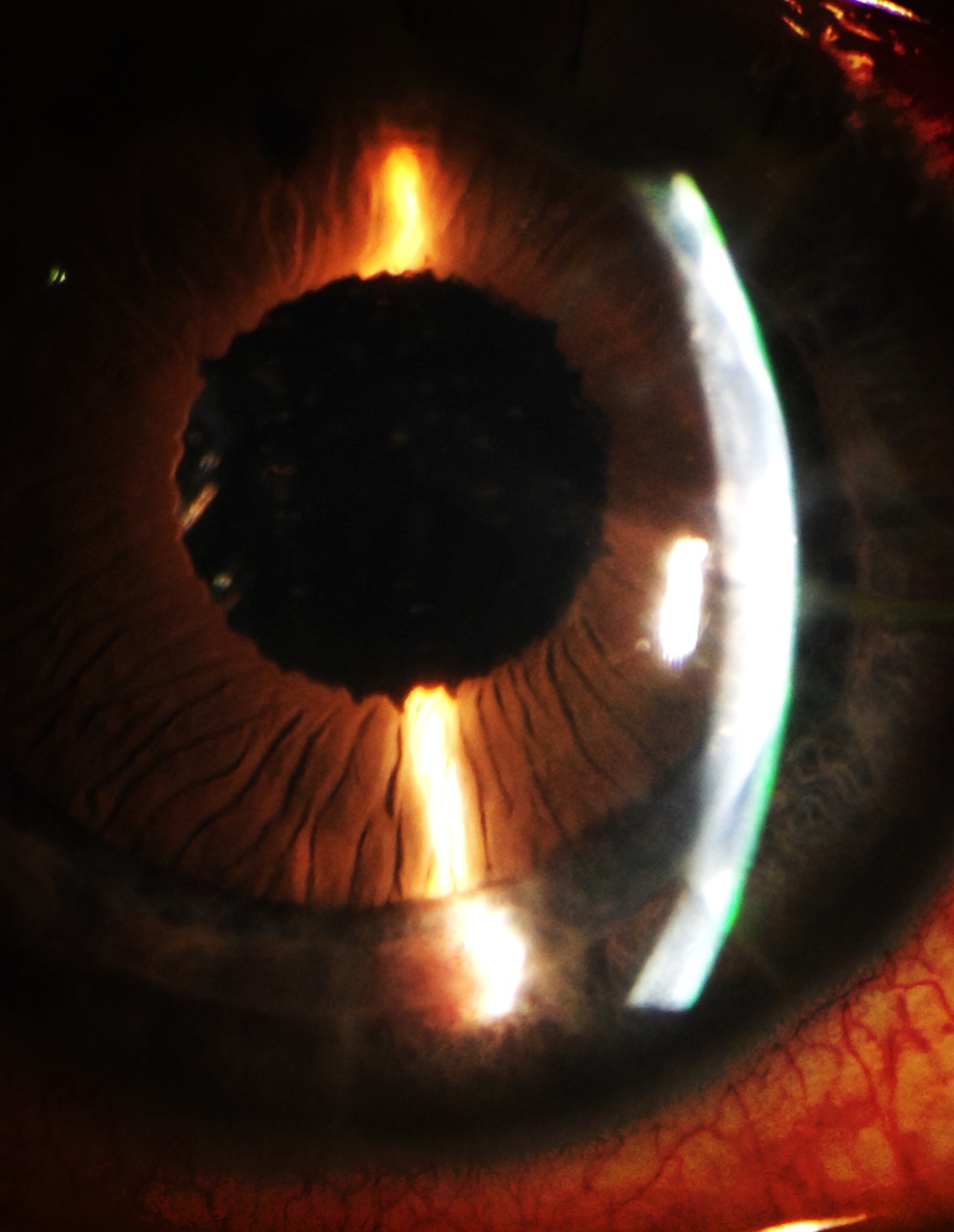
INTRACORNEAL RING REMOVAL 4 YEARS LATER
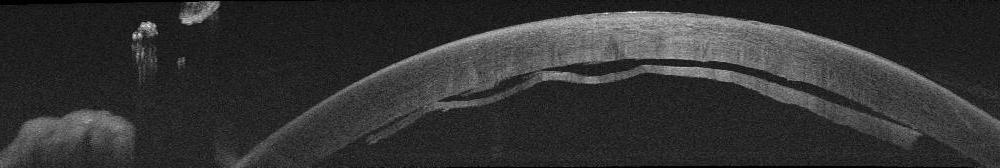
Challenging removal of a fibrotic and vascularised intracorneal segment. Four year after te implantation, the patient reports a white growing spot in the cornea. The Keraring is partially vascularised and covered by a fibrous tissue but not extruded. We tried several maneuvers to remove it, pulling from the hooked hole with an inverted simskey, pushing the distal area, or trying to dissect the primary incision… all of them useless. The only way to do it is looking at the previous records, making a new incision 2 mm from the end of the segment at the depthness set in the initial surgical plan and dissect with a blunt instrument over and under the segment, to refresh the tunnel and pull from one of the sides. No need of specific instruments, buy just in case, fill the tunnel with antibiotic and suture the incisions…